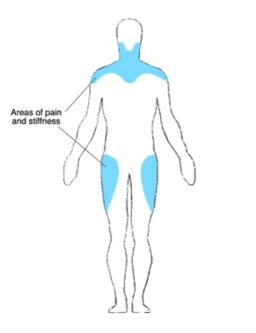
PolyMyalgia Rheumatica (PMR) is an inflammatory condition that causes aching, pain and stiffness in muscles. It typically affects the muscles around the neck, shoulder and hip girdles.
In a small number of cases, approximately 10% of patients with PMR may also develop Giant Cell Arteritis (GCA).
The cause of PMR is unknown, though environmental and genetic factors play a role.
Classically it affects patients over 50 years old, with the biggest peak in those aged 70- 80 years. PMR most commonly affects people of north European ancestry, but can occur in any ethnic group. Women are twice as likely to be affected than men.
PMR often comes on over a period of 1- 2 weeks; sometimes this can be associated with a flu-like illness prior to developing PMR.
Muscle weakness does not characteristically occur in PMR, examination usually shows normal muscle power and function, although limited by pain.
Additional symptoms suggesting Giant Cell Arteritis include
If any of the GCA symptoms are present- you should contact your GP urgently.
There are no definitive tests for PMR. Diagnosis is based on symptoms, raised blood inflammation markers (ESR and CRP) and response to treatment.
Prior to diagnosis a number of tests will be carried out to exclude other causes, these tests include:
Usually PMR is diagnosed and managed by GP’s.
The rheumatology team would usually see cases that are difficult to diagnose, or for symptoms that don’t respond as expected to treatment. Often an Ultrasound of the shoulders is carried out to look for evidence of bursitis- inflammation in the fluid sacks around the shoulder joint.
If giant cell arteritis (GCA) is suspected further tests will be arranged with review in the rheumatology clinic (see link)
PMR is treated by a steroid tablet called Prednisolone. This is started at a dose of 15mg daily and should lead to a rapid control of symptoms within 3-5 days.
Once the symptoms have been controlled the dose of prednisolone will be gradually reduced down over several months as per the recommendation below:
Blood markers for inflammation (ESR and CRP) are checked before each steroid dose reduction to ensure disease control. Typical treatment lengths are around 18 months.
Should symptoms relapse on prednisolone, Blood inflammation markers are usually checked and steroid doses increased and often more slowly reduced.
As prednisolone has a number of side effects, which are discussed on our medication page, medications to help protect the lining of the stomach and prevent osteoporosis may be commenced at the same time.
It’s important never to stop prednisolone tablets suddenly.
In a very small number of patients we need to consider a steroid sparing agent, this would usually be in the form of a DMARD.
Versus Arthritis: http://www.versusarthritis.org