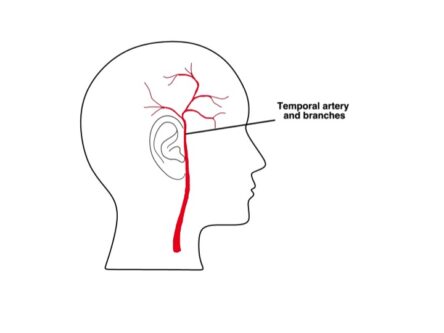
Giant cell arteritis (GCA) is a condition in which inflammation is present in blood vessels called arteries. The inflammation of a blood vessel is called ‘vasculitis’ or arteritis. GCA commonly affects the medium and larger blood vessels that supply the head and neck.
Typically the temporal artery is affected – there is one under the skin on each side of the forehead (the temple area). For this reason, the condition is sometimes called Temporal Arteritis.
Several large arteries may be affected at the same time, which has an impact on the symptoms that are experienced. Rarely, the vasculitis can result in strokes.
GCA is one of the commonest types of vasculitis. It is an inflammatory disease, meaning the body’s immune system inappropriately attacks the health blood vessels.
The exact cause of GCA is unknown, but a person’s genes and factors in the environment play a part.
GCA typically affects people older than 50 years. It is also more common in women than men and in people of Northern European extraction.
A doctor will consider the diagnosis of GCA in a patient that has some of the following symptoms:
General symptoms
Headache
Temporal and scalp tenderness
Jaw claudication
Polymyalgia Rheumatica (PMR)
Visual disturbance
Other symptoms
Urgent medical care should be sought if you have visual changes or symptoms of jaw claudication to prevent permanent blindness or stroke.
GCA is diagnosed based on symptoms, raised inflammatory markers (ESR and CRP) and response to treatment. It is important to start treatment straight away to prevent any serious problems.
Investigations:
If other blood vessels are suspected to be involved a CT scan is often arranged to look for abnormalities in the blood vessel walls in the chest or abdomen.
Previously temporal artery biopsies used to be performed frequently. This is no longer the case as they can often miss the abnormal areas in the blood vessels and would not affect the decision to treat. We are now moving more towards using ultrasound to confirm the diagnosis. Biopsies are more commonly carried out if your symptoms are predominantly related to visual changes.
If GCA is suspected, treatment is usually started straightaway, with a steroid tablet called prednisolone. To minimise delay, prednisolone will be started before some investigations and review by the Rheumatology team which will reduce the risk of complications, including blindness.
Once the symptoms have been controlled (usually within a few days) the dose of prednisolone will be gradually reduced down over several months as per the recommendation below:
Blood markers for inflammation (ESR and CRP) are checked before each steroid dose reduction to ensure disease control. Typical treatment lengths are around 12-18 months.
Should symptoms relapse on prednisolone, blood inflammation markers are usually checked and steroid doses increased and often more slowly reduced.
As prednisolone has a number of side effects, which are discussed on our medication page, medications to help protect the lining of the stomach and prevent osteoporosis are usually commenced at the same time.
In some patients with resistant disease or where it is not possible to reduce the dose of prednisolone to an acceptably low level, there are other drugs that may be considered, such as DMARDs or a biological therapy such as Tocilizumab.
Versus Arthritis: http://www.versusarthritis.org
Vasculitis UK: http://www.vasculitis.org.uk