Osteoarthritis
What is Osteoarthritis (OA)?
Osteoarthritis (OA) is the commonest form of arthritis. It is often referred to as ‘wear and tear damage’. It causes pain and stiffness in the joints.
Symptoms of Osteoarthritis
The symptoms can be variable between patients and are not strictly related to the degree of the X-ray changes.
Symptoms include:
- Pain or discomfort when moving an affected joint
- Increased stiffness of the joint especially after rest, called inactivity gelling
- The joint is no longer a normal shape
- Abnormal crunching sounds from the affected joint
Causes of Osteoarthritis
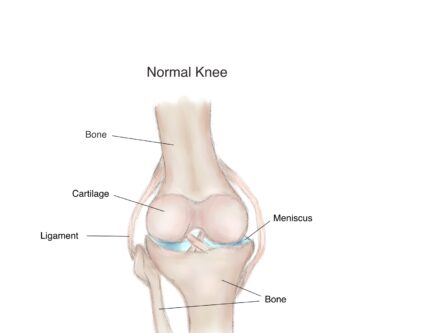
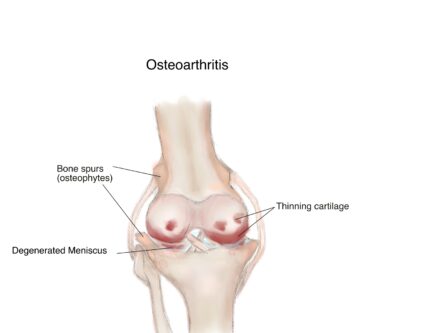
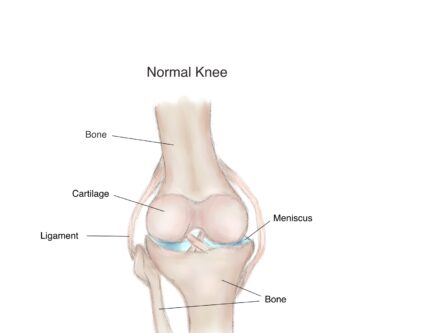
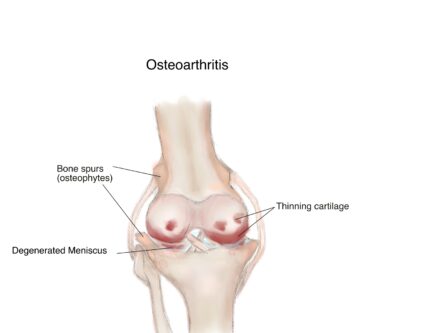
Cartilage is usually a smooth supple material that covers the ends of bones within joints that move. It allows the bones to move within the joint with minimal friction. In OA, the cartilage becomes thinner and rough. This causes the forces that pass through the joint to alter, leading to the crunching sound in the joint on movement and some restriction in joint movement. The bones can change shape and thicken in places, forming bony spurs called osteophytes. The lining of the joints and surrounding tendons (called the synovium and tenosynovium respectively), can become inflamed from time to time. This leads to joint swelling which usually settles down quickly.
It is still not known what causes OA.
Risk factors that to developing Osteoarthritis
Certain risk factors can increase your chances of developing osteoarthritis.
- Age
- OA usually occurs over the age of 45 years. In the UK, at least a third of people above the age of 45 years will develop OA at some point in their lives.
- Weight and obesity
- Being overweight is an important rick factor in causing OA, particularly in weight bearing joints such as the back, hips and knees.
- Joint abnormalities
- Injuries leading to damage in the joint are associated with OA in later life. Normal exercise and activity does not though. If you were born with a joint abnormality (e.g. Perthe’s disease) or have damage from inflammatory arthritis, risk of developing OA is higher.
- Genetic factors
- Genetic factors have a small but important role to play. For example Nodal OA that affects the fingers of middle aged females often runs in families, though the affected genes have not been identified.
How do we diagnose Osteoarthritis?
Your doctor will take a history of the problems you have experienced and examine your joints to arrive at this diagnosis.
X-rays can be helpful in delineating the damage.
Treatment
There is no cure for osteoarthritis but changes to lifestyle, exercise, and pain killers can make it more manageable.
Exercise
- Physical activity helps strengthen muscles and improves pain levels
- A physiotherapist can advise on joint strengthening exercises to help build up muscles if you are unsure
Weight management
- Reducing weight should improve symptoms
Pain relief
- NSAIDs (Non Steroidal Anti- Inflammatory Drugs) like ibuprofen/ diclofenac based gels/ creams can be used. Capsaicin gel can also be beneficial.
- Painkillers like paracetamol can be used regularly.
- Very occasionally if the joint is swollen your doctor may suggest a short course of anti-inflammatory medication or an injection of steroid into the joint. These medications have side effects which means they should not be taken routinely.
Others
- Warm and cold packs can ease pain and swelling in the joints
- Comfortable shoes and insoles can help reduce the strain on joints
- Splints might be helpful for certain joints like the thumb and wrist
- Walking aids may be helpful for some
Surgery
- Should conventional methods not be helpful and there is increased loss of function, joint replacement can be considered for certain joints like the hips or knees. Your GP or doctor can refer you to an orthopaedic surgeon for assessment if this is required.
Useful Links
Versus Arthritis: http://www.versusarthritis.org