Psoriatic arthritis is a chronic inflammatory disease that usually affects those that have Psoriasis. Psoriasis a skin condition causing a red, raised flaky rash that most commonly affects the knees, elbows and scalp. Around 10-20% of people with psoriasis go on to develop arthritis, although some patients develop arthritis before the psoriasis.
Inflammation is a response of the body to injury or infection. It is driven by the immune system. In PsA and psoriasis, cells from the immune system migrate to joints and the skin and become activated, which leads to inappropriate inflammation, skin changes and eventually joint damage. As the immune system cells appear to target healthy tissue, Psoriasis and PsA are known as autoimmune diseases.
As both psoriasis and psoriatic arthritis are autoimmune diseases, around 40% of patients with PsA have a first degree relative with either the skin or joint disease.
There is currently research looking into the role of triggers of developing PsA, such as the gut microbiome (bacteria in the gut), infections, trauma and stress.
Patients who are overweight or smoke are more likely to develop PsA.
PsA is associated with developing other autoimmune disorders
such as inflammatory bowel disease (Crohn’s colitis and Ulcerative colitis) as well as inflammatory eye disease such as uveitis.
Psoriatic arthritis can involve the peripheral joints- joints in the arms or legs or the axial skeleton (spine), where it is part of the group of diseases called spondyloarthropathies.
Skin conditions:
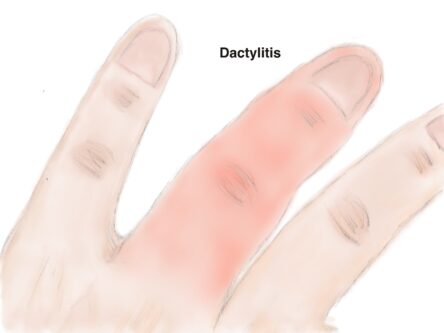
Peripheral joint pain, stiffness and swelling
Back symptoms- Spondylititis
Other rarer symptoms
Metabolic co-morbidities
As PsA is a seronegative disease (no antibodies present), therefore diagnosis is based on symptoms and examination.
Blood tests:
Imaging
Peripheral joints
The mainstay of treatment with Disease-modifying anti-rheumatic drugs (DMARDs).
During acute flares of the joints and whilst the DMARDs take effect we often prescribe a short course of steroids
Drugs such as painkillers may also be prescribed to help reduce the pain. These are good for relieving symptoms but have no effect on progression of the disease.
Biological DMARDs are prescribed as second line therapy if DMARDs fail to control inflammation.
Spondyloarthritis
Non steroidal anti-inflammatories are our first line treatment for back symptoms alone. Should these not improve symptoms or be contraindicated, biological DMARDs would be second line therapy.
Assessment of disease activity
PsARC- For peripheral joints
BASDAI- for spinal symptoms
BSA- body surface area of psoriasis
LES- Leeds enthesitis score (out of 6)
Versus Arthritis: http://www.versusarthritis.org